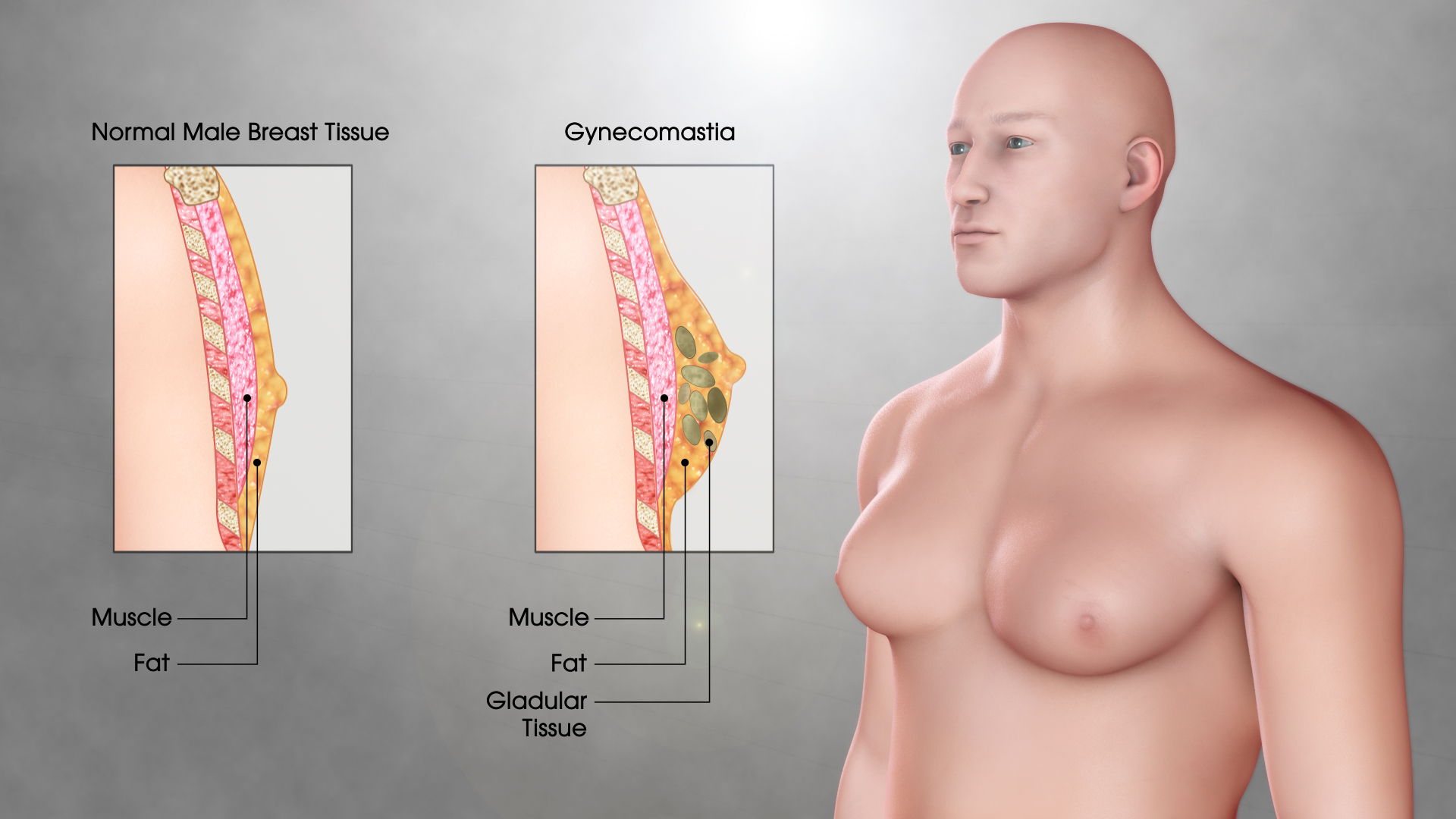
Enlargement of one or both mammary glands in children or men, caused by non-neoplastic proliferation of glandular tissue, sometimes with hypertrophy of adipose tissue. The exclusive growth of adipose tissue is called lipomastia (pseudoginecomastia).
https://www.youtube.com/watch?v=2EtChfouHgI&feature=youtu.be
Ethiopathogenesis and causes
- increased concentration of free (biologically active) estradiol in relation to free blood testosterone caused by:
- increased estrogen biosynthesis during puberty (physiologically), or by testicular tumors producing estrogens or gonadotropins, in adrenal hyperplasia or in adrenal tumors.
- decreased androgen biosynthesis (in hypogonadism or in elderly men).
- increased hepatic production of sex hormone binding globulin (SHBG, eg in hyperthyroidism).
- slowing down the estrogen and androgen metabolism (eg in liver cirrhosis or chronic renal failure).
- increased local activity of aromatase (enzyme that converts testosterone to estradiol), p. ex. in obesity.
- excessive sensitivity of the mammary gland to estrogen.
- congenital androgen receptor defect or its blockage by exogenous agents, e.g. ex. by antiandrogenic drugs (spironolactone, ketoconazole, enalapril, verapamil, ranitidine, omeprazole).
Distribution by age of onset and by the most common causes:
- in children aged 13-14 years: pubertal gynecomastia
- in adult men: persistent gynecomastia since puberty, idiopathic, drug-induced or as a symptom of hormonal disorders or other diseases (symptomatic gynecomastia), p. ex. neoplasm
- gynecomastia in elderly men, due to hormonal or symptomatic changes.
Diagnosis
- History and physical examination: history of drug use. Determine the rate of increase of the mammary glands, the presence of pain and the sensation of tension of the breasts. Carefully examine the mammary gland (texture, elasticity, mobility of the glandular tissue in relation to the adjacent tissue; secretion by any of the nipples), testicles, external genitalia and peripheral lymph nodes. Inquire about the presence of symptoms of hyperthyroidism, hypercortisolism, liver and kidney failure and CNS tumors.
- Complementary explorations
- laboratory tests: blood count, liver and kidney function tests, estradiol concentrations, total testosterone, prolactin, FSH, LH and serum TSH; tumor markers in case of germ cell tumors.
- imaging tests: mammography (if technically possible), ultrasound of both breasts (to exclude breast neoplasia and differentiate gynecomastia from lipomastia) and testicular (search for tumor), in the case of suspected endocrine tumors: ultrasound , CT or adrenal MRI, pituitary MRI, chest x-ray.
- breast biopsy: in case of suspicion of breast cancer (especially if the tumor is unilateral, it can be seen fixed to adjacent tissues and has an irregular structure).
Treatment
Pubertal Gynecomastia Surgery in India in general has a spontaneous regressive course, so in most cases evolution should be observed, without requiring specific therapy. In the adult, if the use of a Gynecomastia causing drug is detect, a modification of the therapy should be evaluated, ideally suspending said drug. If there is hypogonadism or hyperthyroidism as a cause, its specific therapy allows to improve the increase in breast volume. A therapeutic alternative in the case of absence of spontaneous regression or associated pain is the use of tamoxifen or aromatase inhibitors. If there is suspicion of malignancy, medical therapy is ineffective, or Gynecomastia significantly interferes with daily activities, it is possible to consider surgical resection of breast tissue.